Information about COVID-19
Table of Contents
 Information about the Coronavirus
Information about the Coronavirus  It's Not Whether You Were Exposed to the Virus. It's How Much
It's Not Whether You Were Exposed to the Virus. It's How Much  Asymptomatic and Pre-symptomatic Carriers
Asymptomatic and Pre-symptomatic Carriers To Fight Covid-19, Don't Neglect Immunity and Inflammation
To Fight Covid-19, Don't Neglect Immunity and Inflammation  Coronavirus Drug and Treatment Tracker new
Coronavirus Drug and Treatment Tracker new Type A Blood - Revised new
Type A Blood - Revised new When 511 Epidemiologists Expect to Fly, Hug and Do 18 Other Everyday Activities Again
When 511 Epidemiologists Expect to Fly, Hug and Do 18 Other Everyday Activities Again  Understand Coronavirus Test Results new
Understand Coronavirus Test Results new List of Symptoms and When to Seek Medical Attention
List of Symptoms and When to Seek Medical Attention  Heating kills coronavirus
Heating kills coronavirus  When and How to Wash Your Hands by CDC
When and How to Wash Your Hands by CDC Drying your hands
Drying your hands Flushing the Toilet May Fling Coronavirus Aerosols All Over
Flushing the Toilet May Fling Coronavirus Aerosols All Over Visiting Grandchildren
Visiting Grandchildren You're a Senior. How Do You Calculate Coronavirus Risk new
You're a Senior. How Do You Calculate Coronavirus Risk new Expecting Students to Play It Safe if Colleges Reopen Is a Fantasy
Expecting Students to Play It Safe if Colleges Reopen Is a Fantasy Older Children Spread the Coronavirus Just as Much as Adults, Large Study Finds new
Older Children Spread the Coronavirus Just as Much as Adults, Large Study Finds new Grocery Shopping
Grocery Shopping How the Virus Spreads - Includes Videos
How the Virus Spreads - Includes Videos The safety problem for restaurants isn’t the dining room. It’s the kitchen
The safety problem for restaurants isn’t the dining room. It’s the kitchen  Cleaning and Disinfection for Households - CDC
Cleaning and Disinfection for Households - CDC Stay 6 Feet Apart May Not Be Enough
Stay 6 Feet Apart May Not Be Enough Do You Need a Pulse Oximeter?
Do You Need a Pulse Oximeter? CDC Recommends Using a Face Covering
CDC Recommends Using a Face Covering Wearing a mask can irritate your face or make it break out.
Wearing a mask can irritate your face or make it break out. A Map of Who Is Wearing Masks in the U.S. new
A Map of Who Is Wearing Masks in the U.S. new The Covid-19 Trackers
The Covid-19 TrackersThere is a reward at the bottom of this page.
Information about the Coronavirus
- The virus is not a living organism, but a protein molecule (DNA) covered by a protective layer of lipid (fat), which, when absorbed by the cells of the ocular, nasal or buccal mucosa, changes their genetic code. (mutation) and convert them into aggressor and multiplier cells.
- Since the virus is not a living organism but a protein molecule, it is not killed, but decays on its own. The disintegration time depends on the temperature, humidity and type of material where it lies.
- The virus is very fragile; the only thing that protects it is a thin outer layer of fat. That is why any soap or detergent is the best remedy, because the foam CUTS the FAT (that is why you have to rub so much: for 20 seconds or more, to make a lot of foam).
- By dissolving the fat layer, the protein molecule disperses and breaks down on its own.
- HEAT melts fat; this is why it is so good to use water above 77 degrees Fahrenheit for washing hands, clothes and everything. In addition, hot water makes more foam and that makes it even more useful.
- Alcohol or any mixture with alcohol over 65% DISSOLVES ANY FAT, especially the external lipid layer of the virus.
- Any mix with 1 part bleach and 5 parts water directly dissolves the protein, breaks it down from the inside.
- Oxygenated water helps long after soap, alcohol and chlorine, because peroxide dissolves the virus protein, but you have to use it pure and it hurts your skin.
- NO BACTERICIDE OR ANTIBIOTIC SERVES. The virus is not a living organism like bacteria; antibodies cannot kill what is not alive.
- Since the virus is not a living organism but a protein molecule, it is not killed, but decays on its own. The disintegration time depends on the temperature, humidity and type of material where it lies.
- NEVER shake used or unused clothing, sheets or cloth. While it is glued to a porous surface, it is very inert and disintegrates only
- -between 3 hours (fabric and porous),
- -4 hours (copper and wood)
- -24 hours (cardboard),
- - 42 hours (metal) and
- -72 hours (plastic).
- But if you shake it or use a feather duster, the virus molecules float in the air for up to 3 hours, and can lodge in your nose.
- The virus molecules remain very stable in external cold, or artificial as air conditioners in houses and cars.
- They also need moisture to stay stable, and especially darkness. Therefore, dehumidified, dry, warm and bright environments will degrade it faster.
- UV LIGHT on any object that may contain it breaks down the virus protein. For example, to disinfect and reuse a mask is perfect. Be careful, it also breaks down collagen (which is protein) in the skin.
- The virus CANNOT go through healthy skin.
- Vinegar is NOT useful because it does not break down the protective layer of fat.
- NO SPIRITS, NOR VODKA, serve. The strongest vodka is 40% alcohol, and you need 65%.
- LISTERINE IF IT SERVES! It is 65% alcohol.
- The more confined the space, the more concentration of the virus there can be. The more open or naturally ventilated, the less.
- You have to wash your hands before and after touching mucosa, food, locks, knobs, switches, remote control, cell phone, watches, computers, desks, TV, etc. And when using the bathroom.
- You have to Moisturize dry hands from so much washing them, because the molecules can hide in the micro cracks. The thicker the moisturizer, the better.
- Also keep your NAILS SHORT so that the virus does not hide there.
- They also need moisture to stay stable, and especially darkness. Therefore, dehumidified, dry, warm and bright environments will degrade it faster.
It's Not Whether You Were Exposed to the Virus. It's How Much
Three factors seem to be particularly important for aerosol transmission: proximity to the infected person, air flow and timing. For more information, see the article below:
It’s Not Whether You Were Exposed to the Coronavirus. It’s How Much. - The New York Times
Asymptomatic and Pre-symptomatic Carriers
Evidence shows that 25% to 45% of infected people likely don't have symptoms, Fauci told ABC's "Good Morning America" on Wednesday.
The US Centers for Disease Control and Prevention estimates 40% of coronavirus transmission happens before people feel sick.
In one study, about 4 in 5 people with confirmed coronavirus in China were likely infected by people who didn't know they had it, according to research published in the journal "Science."
The CDC said almost half of the 712 people with coronavirus who were on the Diamond Princess cruise ship didn't have any symptoms when they tested positive.
And a study from Iceland showed 50% of those who tested positive had no symptoms at the time of testing.
A study published Tuesday by the CDC on an outbreak aboard the USS Theodore Roosevelt that infected 1,100 crew members provided scientists with a critical test case into the asymptomatic and close-quarters spread of covid-19 among a relatively healthy and young population. The CDC study of 382 young adult service members aboard in April found that 1 in 5 who tested positive reported no symptoms, while those who took preventive measures, such as face coverings and social distancing, reduced their risk of contracting the coronavirus.
Another paper published last week in the Annals of Internal Medicine reviewed 16 of the most relevant studies of asymptomatic infection. It found a likely rate of 40 to 45 percent of those infected don’t have symptoms. But that paper concluded that every study on the subject has been “imperfect in many ways.” One problem is relying on patients to report symptoms because they are not always aware that the tickle in their throat, for instance, is the onset of the virus.
From the Washington Post Are asymptomatic people spreading the coronavirus?
An important finding of this report is that more than half the residents of this skilled nursing facility (27 of 48) who had positive tests were asymptomatic at testing.
From the The New England Journal of Medicine Asymptomatic Transmission, the Achilles’ Heel of Current Strategies to Control Covid-19
To Fight Covid-19, Don't Neglect Immunity and Inflammation
Those factors are immunity, which should be boosted, and inflammation, which should be suppressed. I’ve touched on both in past columns, but now that months of pandemic-related restrictions have impacted the lives of millions, and after seeing who is most likely to become infected and die, immunity and inflammation warrant further discussion and public attention.
One fact is indisputable: Older people are especially vulnerable to this disease and its potentially fatal consequences. But “older” doesn’t necessarily mean “old.” While people over 80 are 184 times more likely to die from Covid-19 than those in their 20s, Dr. Nir Barzilai, scientific director of the American Federation for Aging Research, points out that vulnerability increases starting around age 55.
Immune defenses decline with age. That is a fundamental fact of biology. For example, with advancing age, natural killer cells, a major immunological weapon, become less effective at destroying virus-infected cells. But it doesn’t mean nothing can be done to slow or sometimes even reverse immunological decline, said Dr. Barzilai, who directs the Institute for Aging Research at Albert Einstein College of Medicine.
At the same time, inflammation in tissues throughout the body increases with age, a fact that helps the coronavirus get into the body, bind to molecules in the nose and lungs, and wreak havoc, Janet Lord, director of the Institute of Inflammation and Ageing at the University of Birmingham in England, explained in a webinar this month.
Fat tissue, for example, increases inflammation and renders overweight people more vulnerable to a Covid infection. Here, too, there are established ways to diminish inflammation and thereby enhance resistance to this deadly disease. The basic weapons, diet and exercise, are available to far more people than currently avail themselves of their benefits. Lifestyle can have a major impact on a person’s immune system, for better or worse, Dr. Lord said.
For more information, see the article below:
To Fight Covid-19, Don't Neglect Immunity and Inflammation - The New York Times
Coronavirus Drug and Treatment Tracker new
Coronavirus Drug and Treatment Tracker - The New York Times
A list of 19 of the most-talked-about treatments for the coronavirus.
Type A Blood - Revised
Having Type A blood was linked to a 50 percent increase in the likelihood that a patient would need to get oxygen or to go on a ventilator, according to the new study. For more information, see the two articles below:
Genes May Leave Some People More Vulnerable to Severe Covid-19
Covid-19 Risk Doesn't Depend (Much) on Blood Type, New Studies new
New studies show that people with Type A blood are not at greater risk of getting sick, as previous studies had suggested.
When 511 Epidemiologists Expect to Fly, Hug and Do 18 Other Everyday Activities Again
[In my opinion it doesn't get any better than a nonpolitical opinion from a diverse group of epidemiologists.]
About 6,000 epidemiologists were invited to participate in the survey, which was circulated to the membership of the Society for Epidemiologic Research and to individual scientists. Some said they were uncomfortable making predictions based on time because they didn’t want to guess the timing of certain treatments or infection data. “Our concern is that your multiple choice options are based only on calendar time,” 301 epidemiologists wrote in a letter. “This limits our ability to provide our expert opinions about when we will feel safe enough to stop social distancing ourselves.”
Epidemiologists say they are making decisions based on publicly available data for their region on things like infections and testing. Before choosing whether to do an activity, they might evaluate whether people are wearing masks, whether physical distancing is possible and whether there are alternative ways to do it. Because there is a chance of a second wave of infections, they say they may become less comfortable with certain activities over time, not more.
All bar graphs from article:
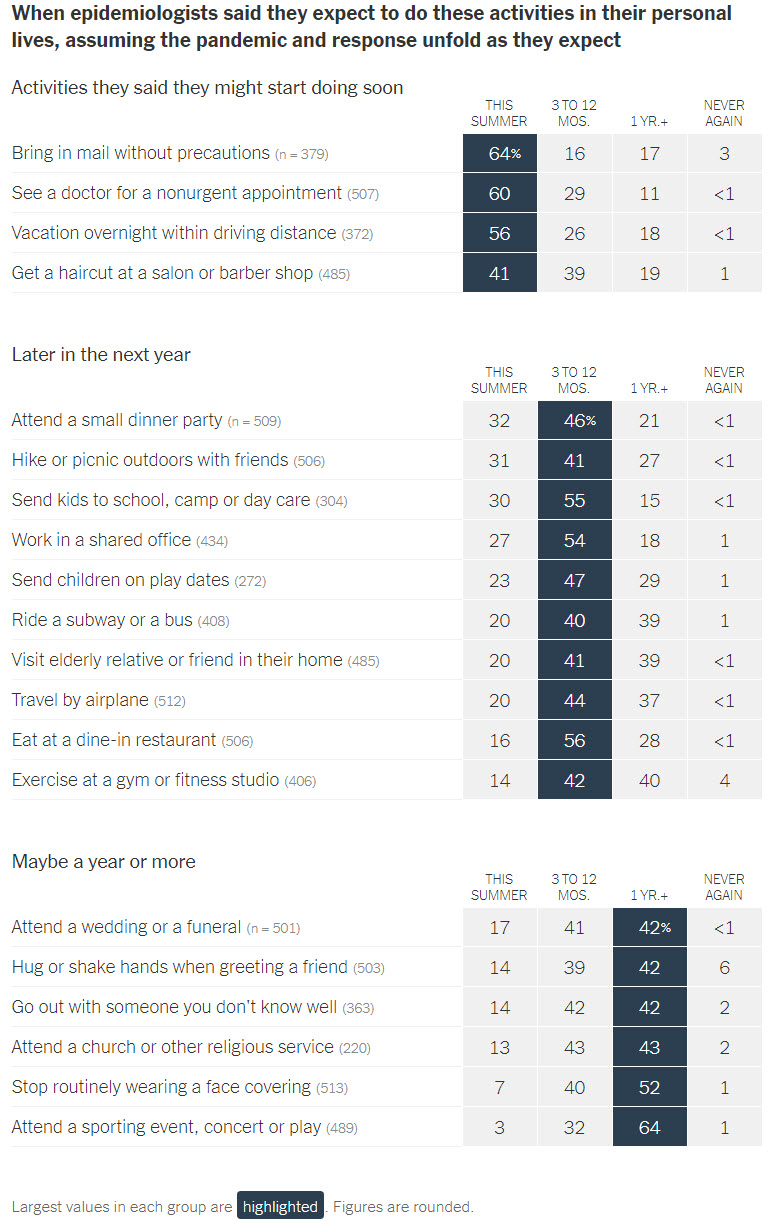
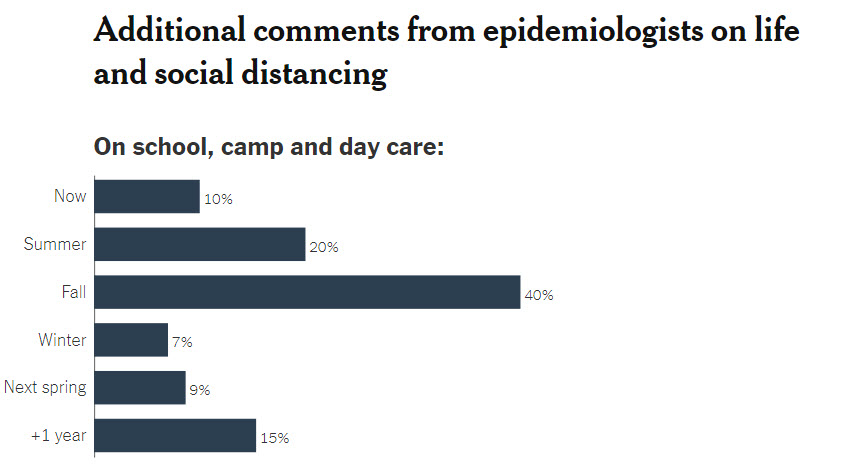
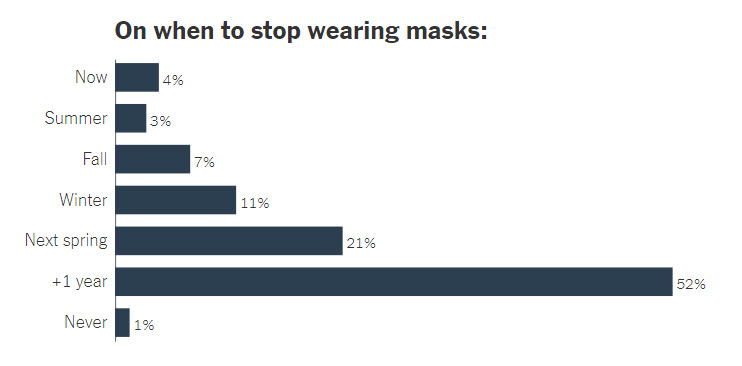
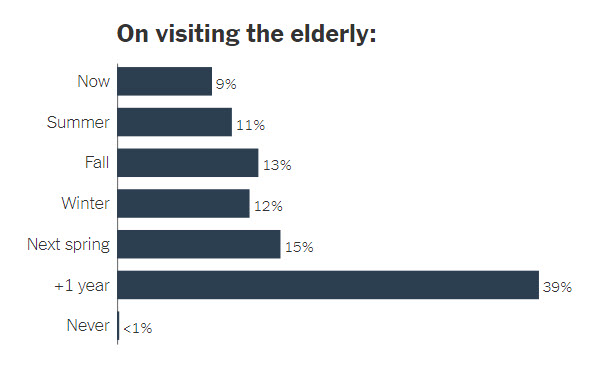
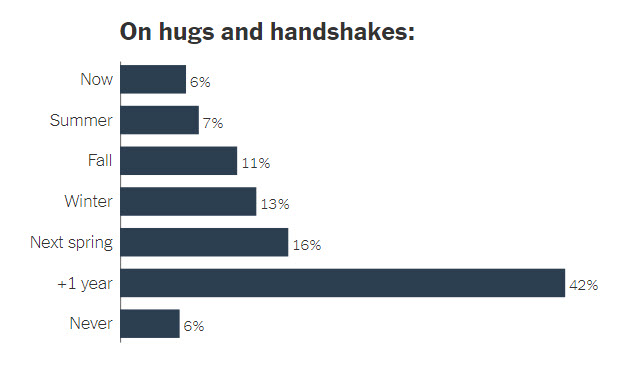
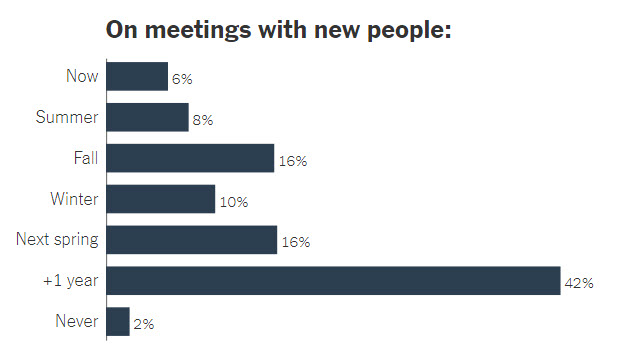
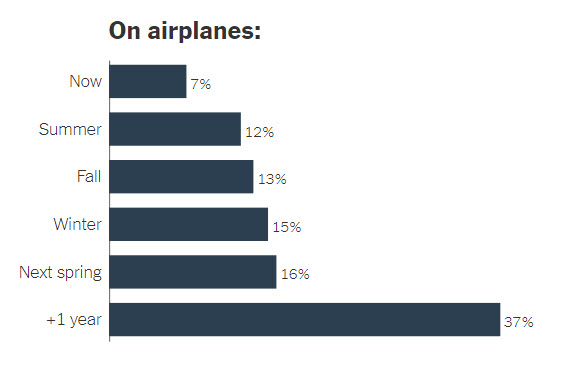
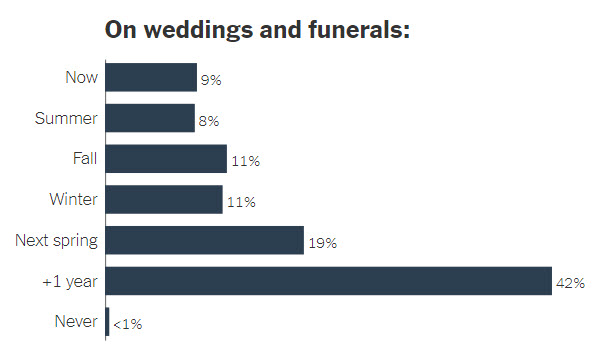
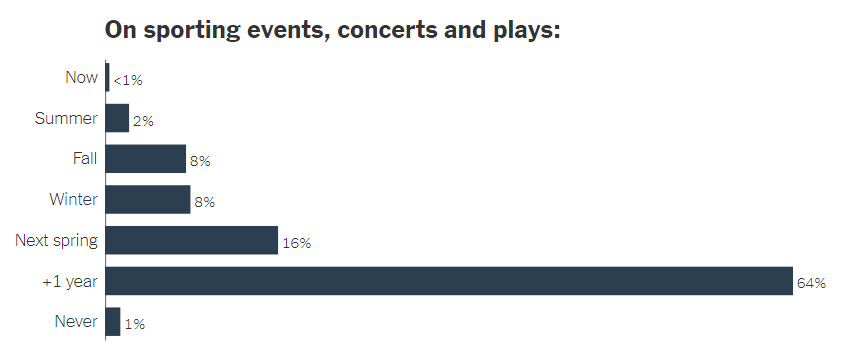 For more information, see the article below:
For more information, see the article below:When 511 Epidemiologists Expect to Fly, Hug and Do 18 Other Everyday Activities Again - NY Times
How to Understand Your Coronavirus Test Results new
It takes time for the coronavirus to replicate to a critical mass for a swabbing test to detect it. The time this process takes varies from person to person and ranges from two to 14 days, experts say.
On average, people tend to show symptoms or test positive for the virus about five days after exposure, Wilson said. Lucy Wilson, an infectious-disease specialist and a professor at the University of Maryland Baltimore County.
As the Atlantic reported last month, it’s still not clear how accurate viral tests are for people who haven’t developed symptoms. There’s a degree of uncertainty, even with a negative test result, and not a lot of data to determine exactly how early a swab test can start to detect the infection for a person showing no symptoms.
Generally, people who have the virus are symptomatic for around six days, Bergstrom said Carl Bergstrom, a University of Washington biology professor who studies infectious diseases.
Antibody tests can also provide a false positive reading, meaning the test indicates you have antibodies from covid-19 when that’s not the case. The false positive may just mean your body has antibodies for another coronavirus, like one that causes the common cold. “We’re just not there yet with the accuracy of the antibody test,” Wilson said.
At the moment, experts can’t say if antibodies from a past covid-19 infection provide someone immunity or even temporary protection from the virus. The virus is still so new. Because of this, Bergstrom said positive antibody tests shouldn’t be used as “a license” to return to the office or other group activities.
For more information, see the article below:
From swabs to antibodies: How to understand your coronavirus test results - Washington Post
Even if a test for Covid-19 is negative, anyone knowingly exposed to the virus is advised to self-isolate for 14 days. And those who develop symptoms consistent with Covid-19 should isolate throughout the entire illness plus three more days after they recover.
The F.B.I. warned last week that scammers were advertising fraudulent antibody tests, and urged those seeking a test to consult the Food and Drug Administration’s website for an approved list of tests and testing companies.
Based on an online report in the journal Nature, Dr. F. Perry Wilson of Yale School of Medicine pointed out that “about 20 percent to 30 percent of people” who recovered from Covid-19 did not have antibody levels significantly greater than those who never were infected.
For more information, see the article below:
The Case for Smarter Coronavirus Testing - The New York Times
List of Symptoms and When to Seek Medical Attention
- CDC - People with COVID-19 have had a wide range of symptoms reported – ranging from mild symptoms to severe illness. These symptoms may appear 2-14 days after exposure to the virus:
Fever, Cough, Shortness of breath or difficulty breathing, Chills, Repeated shaking with chills, Muscle pain, Headache, Sore throat and/or New loss of taste or smell
- If you have any of these emergency warning signs for COVID-19 get medical attention immediately: Trouble breathing, Persistent pain or pressure in the chest, New confusion or inability to arouse, Bluish lips or face. This list is not all inclusive. Please consult your medical provider for any other symptoms that are severe or concerning to you. Call 911 if you have a medical emergency: Notify the operator that you have, or think you might have, COVID-19. If possible, put on a cloth face covering before medical help arrives.
Link to CDC's Symptoms page
- World Health Organization (WHO) List of Symptoms: The most common symptoms of COVID-19 are fever, dry cough, and tiredness. Some patients may have aches and pains, nasal congestion, sore throat or diarrhea.
Link to WHO's Symptoms page - If you have any of these emergency warning signs for COVID-19 get medical attention immediately: Trouble breathing, Persistent pain or pressure in the chest, New confusion or inability to arouse, Bluish lips or face. This list is not all inclusive. Please consult your medical provider for any other symptoms that are severe or concerning to you. Call 911 if you have a medical emergency: Notify the operator that you have, or think you might have, COVID-19. If possible, put on a cloth face covering before medical help arrives.
Heating kills coronavirus
- If used properly, moderate or high heat can be used to "kill" coronavirus, inactivating the virus so that it is no longer infectious. However, this can be more time-consuming than other methods such as chemical disinfection (with disinfecting wipes or sprays) and there is often no need to disinfect packaging at all if you can just remove the packaging, dispose of it (preferably by recycling), and then disinfect your hands by washing with soap and warm water or using another disinfection method.
- Heat is very effective at disinfecting objects from coronavirus. Experiments done in China on the coronavirus SARS-CoV (Duan, Biomed Env Sci 2003), which is similar to the SARS-CoV-2 that causes COVID-19, found that coronavirus was completely deactivated (essentially sterilized) within 30 minutes when subjected to a temperature of 167 degrees Fahrenheit. It took 60 minutes at 152 degrees and 90 minutes at 132 degrees. At 99 degrees or lower, the virus remained quite infectious at two hours, when the experiment ended.
- This suggests, for example, that if you purchase take-out food and wish to disinfect the container itself of coronavirus (as well as keep your food warm), you can simply place the container in a warm (150 degree) oven or warming drawer for an hour to disinfect it. Just be sure it is not directly exposed to a heating element so as not to pose a fire hazard. Most plastic and paper containers are stable for short periods at 150 degrees.
- Heating a face mask this way may also disinfect it, and a study by researchers at Stanford University found that heating N95 masks at 167 degrees for 30 minutes did not compromise the masks, even after 20 cycles.
- Don't directly refrigerate — it keeps the virus infectious
- Heat is very effective at disinfecting objects from coronavirus. Experiments done in China on the coronavirus SARS-CoV (Duan, Biomed Env Sci 2003), which is similar to the SARS-CoV-2 that causes COVID-19, found that coronavirus was completely deactivated (essentially sterilized) within 30 minutes when subjected to a temperature of 167 degrees Fahrenheit. It took 60 minutes at 152 degrees and 90 minutes at 132 degrees. At 99 degrees or lower, the virus remained quite infectious at two hours, when the experiment ended.
- What this and other research suggest is that you should not place a recently purchased food container directly into a refrigerator and you should not "quarantine" a recently received package in a cold cellar or cold garage, as this will preserve coronavirus and could keep it infectious for days.
Link to Consumer Lab
When and How to Wash Your Hands by CDC Link to CDC Instructions
Drying your hands after washing is a key part of coronavirus prevention
- Anna Medaris Miller, Business Insider USMarch 9, 2020
- Washing your hands frequently and thoroughly is one of the most important ways to protect yourself and others from the novel coronavirus.
- But drying your hands properly is just as important since wet or moist hands can breed germs.
- Different drying methods have different levels of effectiveness, with paper towels being one of the best and air dryers being the worst, a hygiene expert told Insider.
- People concerned about coronavirus outbreaks have heard the message loud and clear: Wash your hands, and wash them well and often.
- But the other half of that public-health message – to dry your hands just as well – is just as important, according to Miryam Wahrman, a biology professor at William Paterson University and the author of “The Hand Book: Surviving in a Germ-Filled World,” which dedicates seven pages to the topic. [see link below]
- “The very act of drying hands is rife with potential problems, problems of the recontamination of hands,” she told Insider. “You do not want to undo the good of handwashing in the process of drying hands.”
- You could do that if your hands stay wet or even just damp, since moisture is precisely what germs thrive on.
The drying method matters, too. The most hygienic way to dry is with paper or cloth towels, Wahrman said.
- “Research studies show that drying with paper towels or cloth towels removes even more germs than washing alone, as the friction of drying reduces the germ count even further,” she said.
- Cloth towels come with more caveats: They should only be used at home, where each person has his or her own towel and spot to hang it, and thrown in the laundry regularly – even every few days if they’re used often.
- Paper towels are just as effective and can also be used to turn off the faucet and open the door, although they’re less environmentally friendly than the cloth variety.
- Warm air or jet air dryers, on the other hand, don’t come recommended by Wahrman. “They can spew germs back on your hands, and into the air where you can breathe them in.”
- Indeed, one study found that air dryers can blow around potentially pathogenic air, even prompting a Connecticut health center to trade their dryers for paper towels in order to help protect people with compromised immune systems, as Business Insider previously reported.
- Plus, if you’re impatient and don’t wait for your hands to dry completely, you’ll again have created an environment in which germs can flourish.
- What’s more, “moist hands touching a public doorknob on the way out of a public bathroom are the perfect storm of recontamination, making your clean hands germ-covered again,” Wahrman said.
- She recommended using paper towels when available in public restrooms, and keeping a few clean tissues in your pocket for the times they’re unavailable.
- Link to Business Insider article
- Link to Miryam Wahrman' book
Flushing the Toilet May Fling Coronavirus Aerosols All Over Another article recommends, when at home, shutting the lid before flushing.
https://www.nytimes.com/2020/06/16/health/coronavirus-toilets-flushing.html
Visiting Grandchildren
Tina Q. Tan, medical director of the international patient services program at the Ann & Robert H. Lurie Children’s Hospital of Chicago and professor of pediatrics at the Northwestern University Feinberg School of Medicine advise ... is to wear a mask and gloves, and stay six feet away. Say hello to them but don’t touch them. No hugs and kisses. Lots of hand-washing and be sure the older person is up to speed on vaccines,” including for influenza, Tdap (tetanus, diphtheria and pertussis) and pneumococcal pneumonia. “If you have to see them, they can’t touch you, and you can’t touch them. I know this is difficult, but even if the kids are staying home, their parents probably aren’t.”
It’s also a good idea to avoid or limit visits to newborns and young infants, experts say, painful advice for a new grandparent.
Still, if grandparents live close to the new baby, and everyone in both households has been self-quarantining, “it’s probably okay to visit,” Malani says. “The main issue is to make sure there hasn’t been any community exposure. (Preeti Malani, an infectious-disease specialist and geriatrician, who also is professor of medicine at the University of Michigan.)
Visiting grandchildren during covid-19 means risk calculation - The Washington Post
The safer strategy is to spend time together outdoors — the risk for viral transmission outside is far lower than inside. Everyone should wash their hands, and stay at least six feet apart. Some experts suggest 10 to 12 feet if the grandparent is a very elderly person or has a chronic health condition. Even outdoors, everyone over the age of 2 — and not just the grandparent — should wear a mask. Children are more likely to wear a mask if you explain to them that it’s to protect someone they love.
Masks can be removed for meals, but everyone should stay at least six feet apart from the older person. Don’t share food or drinks — it increases the risk of close contact or catching germs from serving utensils and dishes. If you have hand sanitizer, use it often. And avoid touching the face.
Remember, the biggest worry is being in an enclosed space with someone who has the virus but doesn’t know it. Keep everyone outside, if possible. But if a child must enter a grandparent’s house, monitor them and allow it only when the grandparent is outside. Everyone should wear a mask, and sanitize the bathroom after use. If the grandparent is visiting you, designate one disinfected bathroom just for them and keep children outdoors.
When Can I See My Grandkids_ - The New York Times
You're a Senior. How Do You Calculate Coronavirus Risk new
Expecting Students to Play It Safe if Colleges Reopen Is a Fantasy
Dr. Steinberg is a professor of psychology at Temple University
Older Children Spread the Coronavirus Just as Much as Adults, Large Study Finds new
In the heated debate over reopening schools, one burning question has been whether and how efficiently children can spread the virus to others. A large new study from South Korea offers an answer: Children younger than 10 transmit to others much less often than adults do, but the risk is not zero. And those between the ages of 10 and 19 can spread the virus at least as well as adults do.
Children under 10 were roughly half as likely as adults to spread the virus to others, consistent with other studies. That may be because children generally exhale less air — and therefore less virus-laden air — or because they exhale that air closer to the ground, making it less likely that adults would breathe it in.
How to Protect Yourself From Coronavirus When Grocery Shopping by Consumer Reports
How the Virus Spreads - Includes Videos
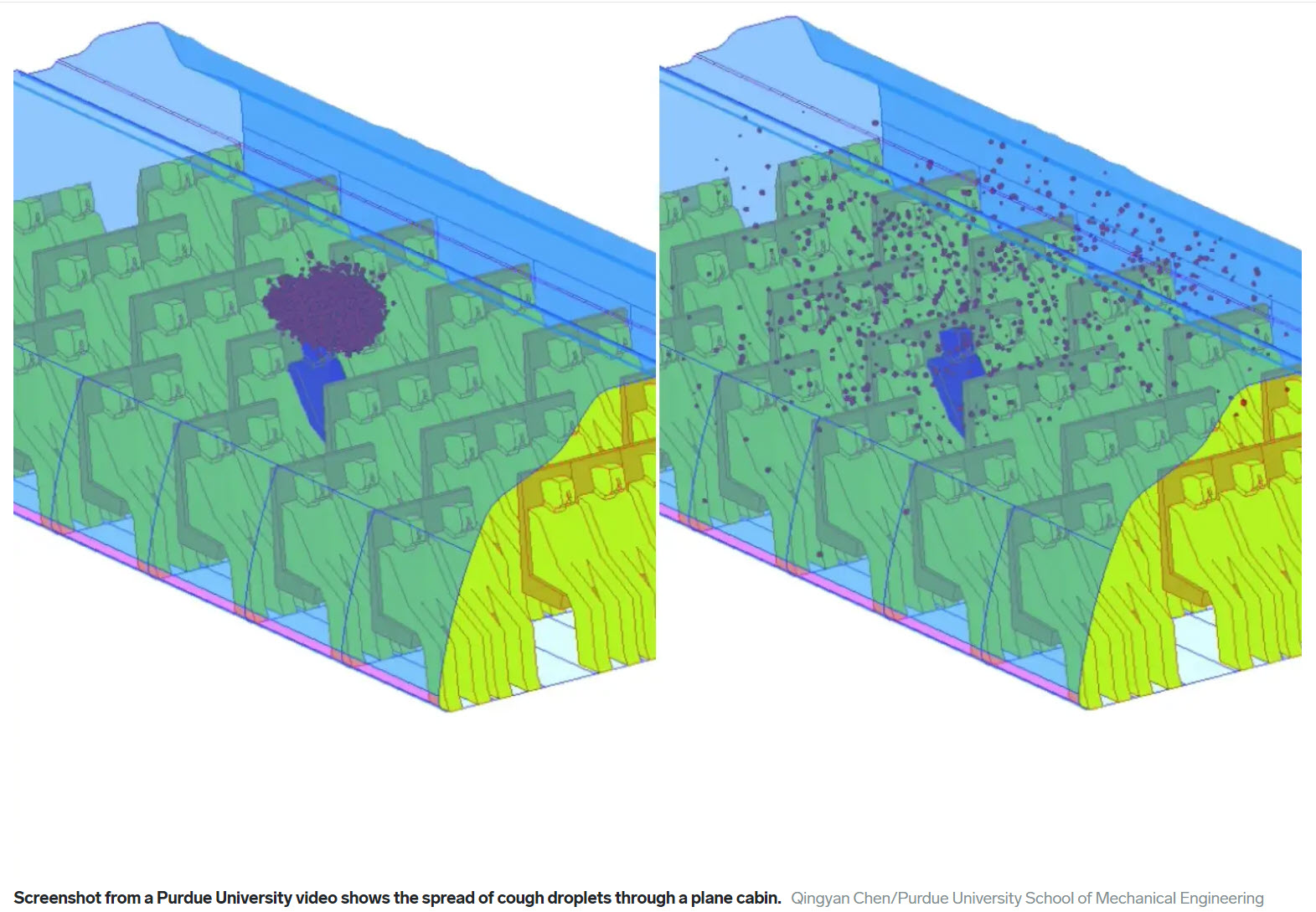
How a single cough can spread invisible droplets throughout a plane cabin - Business Insider
Black Light Experiment Shows How Quickly COVID-19 Can Spread - YouTube
A public broadcaster NHK conducted and filmed a test to show how easily and quickly viruses like COVID-19 can spread in public. Invisible fluorescent paint was applied to the hand of one person. 10 participants then served themselves at a makeshift buffet and ate for 30 minutes. Afterwards, a black light revealed how far and wide the paint had traveled.
See how quickly flu germs spread in a classroom - ABC News
New Facts about Infection Mechanisms - speaking to another person - YouTube
The safety problem for restaurants isn’t the dining room. It’s the kitchen
...Chefs and other kitchen staff are quietly raising the alarm about the prospect of returning to what once passed for normal: chaotic, overcrowded, poorly ventilated kitchens where everyone is shouting, everyone is touching multiple surfaces and nobody has time for safety precautions when the front of the house gets slammed. “We’re touching food. We’re in close contact. There’s no social distancing,” says Michelle DeChesser, 52, a 20-year kitchen veteran who has worked as a chef at upscale restaurants from Portland, Ore., to Lancaster, Pa.
The safety problem for restaurants isn’t the dining room. It’s the kitchen. - The Washington Post
Cleaning and Disinfection for Households - CDC
For disinfection, most common EPA-registered household disinfectants should be effective. A list of products that are EPA-approved for use against the virus that causes COVID-19 is available here:
List N: Disinfectants for Use Against SARS-CoV-2 - EPA updates this site with new data.EPA data rearranged I took the EPA data (as of 5/7/20) and arranged it in a more user friendly format that can be easily printed.
Beyond Pesticides - Disinfectants and Sanitizers They believe that cleaning and disinfecting should reduce risk from pathogens, but if materials are not used properly, they can actually increase risk.
Beyond Pesticides Guide for Residential Use A guide on what to look for when buying disinfectants and sanitizers selected from the EPA list above. Updated 5/8/2020. Check the disinfectant you want to use against there website (above) for the latest information.
Stay 6 Feet Apart. Simulated Cough Reveals That May Not Be Enough
A video showing how far a cough or sneeze goes in the air.
These days, even the sound of a cough – one of the most common symptoms of the coronavirus disease (COVID-19) – can cause panic and fear. People can get infected when a person coughs or sneezes as tiny droplets travel and permeate the air. These particles can land on surfaces, in a person’s mouth, nose or eyes or can be breathed in by someone nearby. Social distancing recommendations inform people to stay 6 feet apart from one another. A preliminary, flow visualization experiment suggests that this may not be sufficient.
Researchers from Florida Atlantic University’s College of Engineering and Computer Science conducted an experiment using flow visualization to demonstrate how far a cough travels and how long it lingers in the air. Flow visualization is a method that enables flow patterns, such as a stream of particles from a cough, to become visible in fluids like air and water since they are transparent. Various techniques using flow visualization make these patterns visible to the naked eye.
In a laboratory setting, the researchers were able to visually demonstrate a mechanically emulated cough/sneeze jet from an orifice representing the mouth and the associated particle-laden airflow using a mannequin and other props.
“Preliminary results from our experiment reveal that significant concentrations of small particles from a turbulent jet such as from a heavy cough/sneeze can linger in still air for more than one minute. It only took the particles a couple of seconds to travel 3 feet; in about 12 seconds it reached 6 feet and in about 41 seconds it reached around 9 feet,” said Siddhartha Verma Ph.D.
For a heavy cough, the researchers found that particles can even travel up to 12 feet. A lighter cough does not travel as far.
Excellent Youtube video and details at http://www.fau.edu/newsdesk/articles/mechanical-cough-coronavirus.php
Do You Need a Pulse Oximeter?

Too many patients were showing up at the hospital with perilously low oxygen levels, putting them at risk for severe complications and death.
But a simple home gadget called a pulse oximeter could help alert patients to seek help sooner, he said.
Dr. Levitan noted that patients with Covid-19 can experience a potentially dangerous drop in oxygen saturation without having obvious breathing problems. Without a pulse oximeter, they might never know it or get very used to how they feel, despite very low oxygen levels. By the time they go to the hospital feeling shortness of breath, their oxygen levels would have dropped significantly, and they could have very advanced Covid pneumonia.
“They are still talking, thinking clearly, and not in obvious distress,” Dr. Levitan said. “If the level of oxygen became this low all of sudden, these patients would be unconscious, having seizures, or otherwise affected. What that means to me is there is a period of days where they were going silently down and they didn’t know it.”
CDC Recommends Using a Face Covering (Link to CDC)
The Best Material for a Mask (NY Times Article summary)
In recent tests, HEPA furnace filters scored well, as did vacuum cleaner bags, layers of 600-count pillowcases and fabric similar to flannel pajamas. Stacked coffee filters had medium scores. Scarves and bandanna material had the lowest scores, but still captured a small percentage of particles.
“Hold it up to a bright light,” said Dr. Scott Segal, chairman of anesthesiology at Wake Forest Baptist Health who recently studied homemade masks. “If light passes really easily through the fibers and you can almost see the fibers, it’s not a good fabric. If it’s a denser weave of thicker material and light doesn’t pass through it as much, that’s the material you want to use.”
The best medical mask — called the N95 respirator — filters out at least 95 percent of particles as small as 0.3 microns. By comparison, a typical surgical mask — made using a rectangular piece of pleated fabric with elastic ear loops — has a filtration efficiency ranging from 60 to 80 percent.
An allergy-reduction HVAC filter worked the best, capturing 89 percent of particles with one layer and 94 percent with two layers. A furnace filter captured 75 percent with two layers, but required six layers to achieve 95 percent. To find a filter similar to those tested, look for a minimum efficiency reporting value (MERV) rating of 12 or higher or a microparticle performance rating of 1900 or higher.
The problem with air filters is that they potentially could shed small fibers that would be risky to inhale. So if you want to use a filter, you need to sandwich the filter between two layers of cotton fabric.
A 600 thread count pillow case captured just 22 percent of particles when doubled, but four layers captured nearly 60 percent. A thick woolen yarn scarf filtered 21 percent of particles in two layers, and 48.8 percent in four layers. A 100 percent cotton bandanna did the worst, capturing only 18.2 percent when doubled, and just 19.5 percent in four layers.
The group also tested Brew Rite and Natural Brew basket-style coffee filters, which, when stacked in three layers, showed 40 to 50 percent filtration efficiency — but they were less breathable than other options.
Tests showed good results for homemade masks using quilting fabric.The best-performing designs were a mask constructed of two layers of high-quality, heavyweight “quilter’s cotton,” a two-layer mask made with thick batik fabric, and a double-layer mask with an inner layer of flannel and outer layer of cotton.
For other mask materials and more details see:
https://www.nytimes.com/article/coronavirus-homemade-mask-material-DIY-face-mask-ppe.html
Wearing a mask can irritate your face or make it break out.
Wearing a mask can irritate your face or make it break out. Here’s what to do about ‘maskne.’ - New York Times
A Map of Who Is Wearing Masks in the U.S. new
A Very Detailed Interactive Map of Who Is Wearing Masks in the U.S. - zoom into your area New York Times
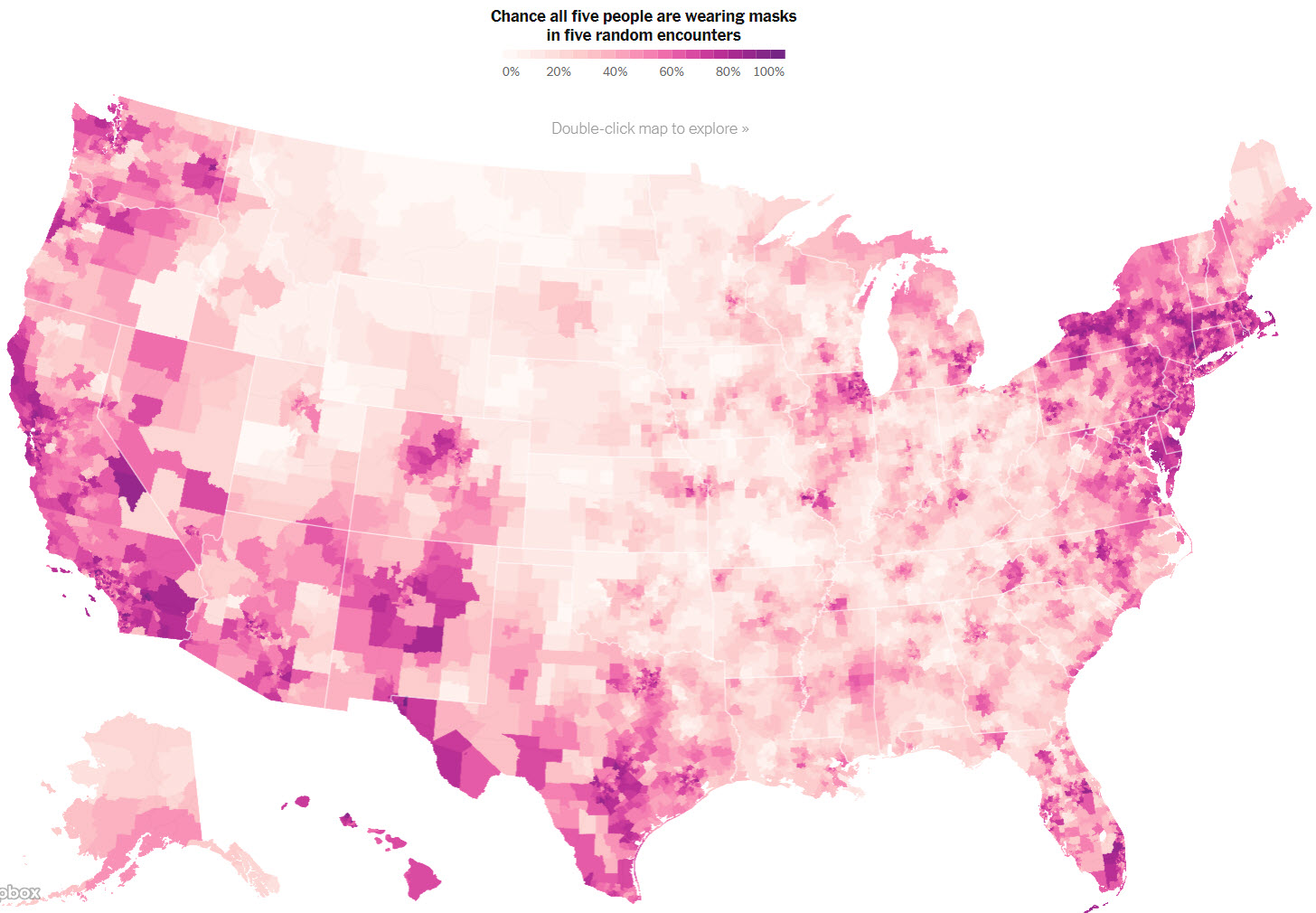
Picture of map above is obviously not interactive.
The Covid-19 Tracker and NY Times Tracker
This website offers a snapshot of the crisis right now. Click on a country name to get a more detailed geographic breakdown at the state, province, or county level. An easy to use and understand website with data (shown in a bar graphs) from the first case to the current time.
https://www.statnews.com/2020/03/26/covid-19-tracker/
The datasets are drawn from the Johns Hopkins University Center for Systems Science and Engineering, from the COVID Tracking Project, and from USAFacts.
The Center for Systems Science and Engineering (CSSE) is a research collective housed within the Department of Civil and Systems Engineering (CaSE) at Johns Hopkins University (JHU)
Summaries, maps and detailed data.
https://www.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
The COVID Tracking Project collects and publishes the most complete testing data available for US states and territories. Our most up-to-date data and annotations
The COVID Tracking Project, launched from The Atlantic, obtains, organizes, and publishes high-quality data required to understand and respond to the COVID-19 outbreak in the United States. This is the spreadsheet version of the COVID Tracking Project dataset.
https://covidtracking.com/data
Coronavirus numbers by state with links to each state agency
https://docs.google.com/spreadsheets/u/2/d/e/2PACX-1vRwAqp96T9sYYq2-i7Tj0pvTf6XVHjDSMIKBdZHXiCGGdNC0ypEU9NbngS8mxea55JuCFuua1MUeOj5/pubhtml#The NY Times Has Five Ways to Follow the Coronavirus Outbreak for Any Metro Area in the U.S.
Just type in your city name and state.
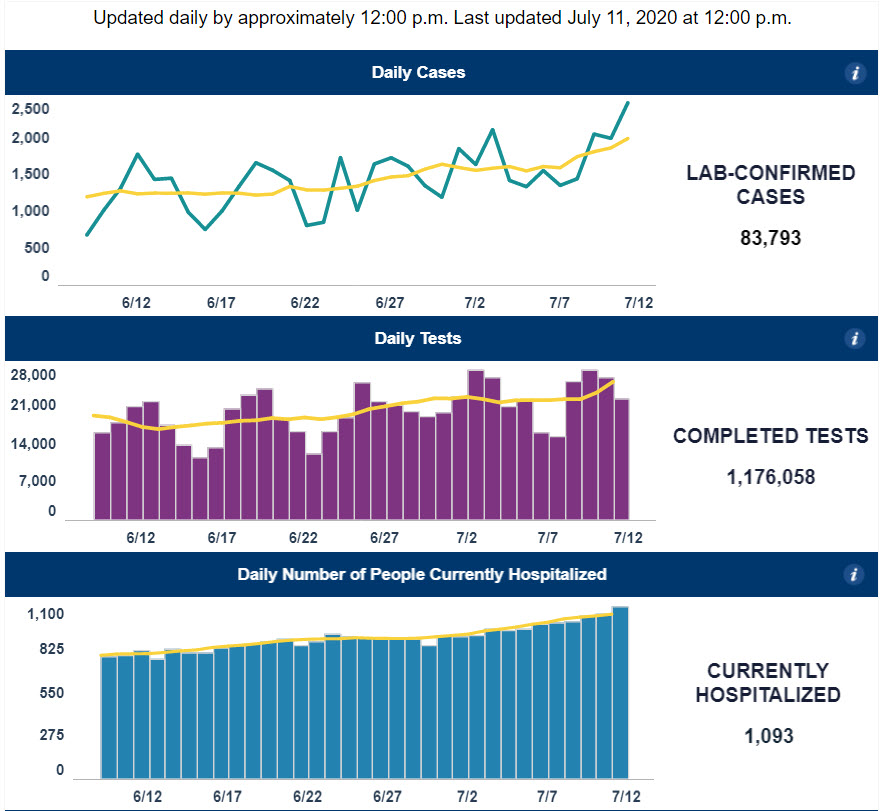
NCDHHS' COVID-19 Response new
North Carolina Department of Health and Human Services - COVID-19 Response - see Dashboard
Example of graphs below (also has maps):
On a personal note:
A friend of mine received the following email from a native German but lives in both countries.
Oh, it is a different world over there, for sure. They have plenty of masks and share with anyone who needs one. I got offers left and right. Not wearing one in public carries a fine of €3000 as posted in some places. They do contact tracing in restaurants. They have tests freely available. Everybody can afford to be tested at the first symptom - not when they are gravely ill. No-one gets turned away. They know that people who get it can get healed. About 98% of them are in Germany!! They also know that people can get the disease more than once. They are treating people who got it a second time! They also know that the antibodies are very ineffective (1,3%) and short-lived. So never mind our musings about immunity, let alone herd-immunity.
Your reward for reading this material
I've been thinking that....
Until further notice the days of the week are now called thisday, thatday, otherday, someday, yesterday, today and nextday!Can we uninstall 2020 and reinstall it again?... I think it has a virus ...
Just asked a 6 year old if he understands why there is no school. He said yes because they are out of toilet paper.
On the bright side, I am no longer calling this shelter-in-place. I am an artist-in-residence.
After years of wanting to thoroughly clean my house but lacking the time, this week I discovered that wasn’t the reason.
Where is your next travel destination?
- Las Kitchenas
- Los Lounges
- Santa Bedroomes
- Porto Gardenas
- Los Bed
- Costa del Balconia
- St Bathroom
- La Rotonda de Sofa
You’re not stuck at home, you’re safe at home. One word can change your attitude and one cough can change your life.
Coronavirus has turned us all into dogs. We roam the house all day looking for food. We’re told “no” if we get too close to strangers and we get really excited about car rides.
If you thought toilet paper was crazy ... just wait until 300 million people all want a haircut appointment.
2020 is a unique Leap Year. It had 29 days in February, 300 days in March and 5 years in April.
If you keep a glass of wine in each hand, you can’t accidentally touch your face.
This cleaning with alcohol is total b.s. NOTHING gets done after that first bottle.
Kinda’ starting to understand why pets try to run out of the house when the door opens.
Does anyone know if we can take showers yet or should we just keep washing our hands???
You think it’s bad now? In 20 years our country will be run by people home schooled by day drinkers….
Day 7 at home and the dog is looking at me like, “See? This is why I chew the furniture.”
My Mom always told me I wouldn’t accomplish anything by laying in the bed all day, but look at me now! I’m saving the world!
I miss the days when we were terrified of Romaine lettuce Ahh, the good times….
I swear my fridge just said: “what the hell do you want now?”
Whoever owes you money, go to their house now. They should be home.
Homeschooling Day #3: they all graduated. #Done.
New monthly budget: Gas $0; Entertainment $0; Clothes $0; Groceries $2,799.
Breaking News: Wearing a mask inside your home is now highly recommended. Not so much to stop COVID-19, but to stop eating.
When this quarantine is over, let's not tell certain people.
I stepped on my scale this morning. It said: "Please practice social distancing. Only one person at a time on scale."
Not to brag, but I haven't been late to anything in over 12 weeks.
They can open things up this month, but I'm staying in until July to see what happens to the rest of you first!
The spread of Covid-19 is based on two things:
1. How dense the population is.
2. How dense the population is.
People keep asking: "Is coronavirus REALLY all that serious?" Well, the churches and casinos closed. When heaven and hell agree on the same thing it's probably pretty serious.
Never in a million years could I have imagined I would go up to a bank teller wearing a mask and ask for money!
Coronavirus has made us start acting like our dogs. We wander around the house looking for food. We get told "No" if we get too close to strangers. And we get really excited about going for walks and car rides!
The dumbest thing I've bought so far is a 2020 planner.